Turn patient-centric with our Prior
Authorization solution to
maximize reimbursements
patient-centric Prior Authorization solution to provide the best experience.
Healthcare Industry Roadblocks

Health insurance approval is time consuming for doctors due to the administrative tasks involved in authorizing prescriptions and convincing insurance companies to bear the cost of the treatment.

The need for specific policies and forms in insurance coverage have increased. This makes it difficult to stay updated with changing needs.

Patients who don’t get timely treatment due to delay in insurance cover understand the real benefits of prior authorization.
Exploring Key Features of Prior Authorization
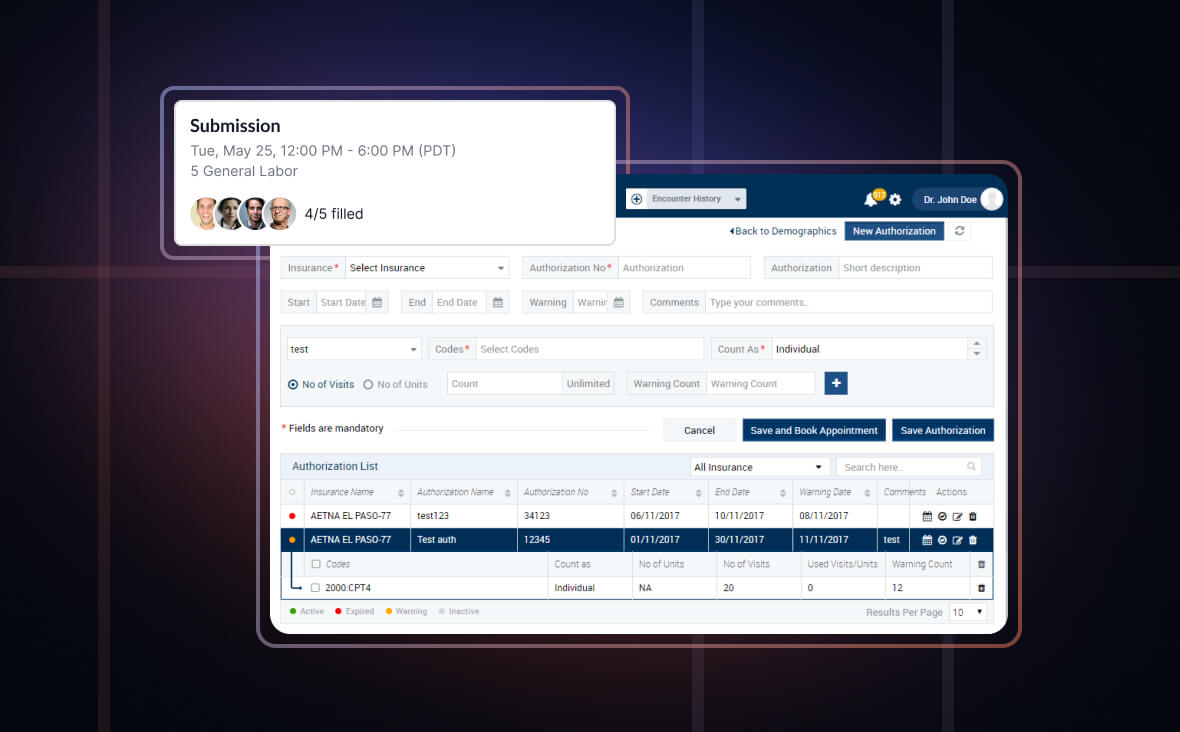
With our prior authorization solution, healthcare providers can send requests to insurance companies electronically which helps get the review and approval easily. It saves time, reduces errors and speeds up the process.
Our solution enables checking for eligibility in real time that helps know the status of the insurance cover, provides precise estimates and avoids delay in treatment.
Our prior authorization solution is integrated with tools that offer clinical guidelines and decision support. Healthcare providers can find out if a particular treatment aligns with the medical guidelines so that the patient will likely get prior authorization.
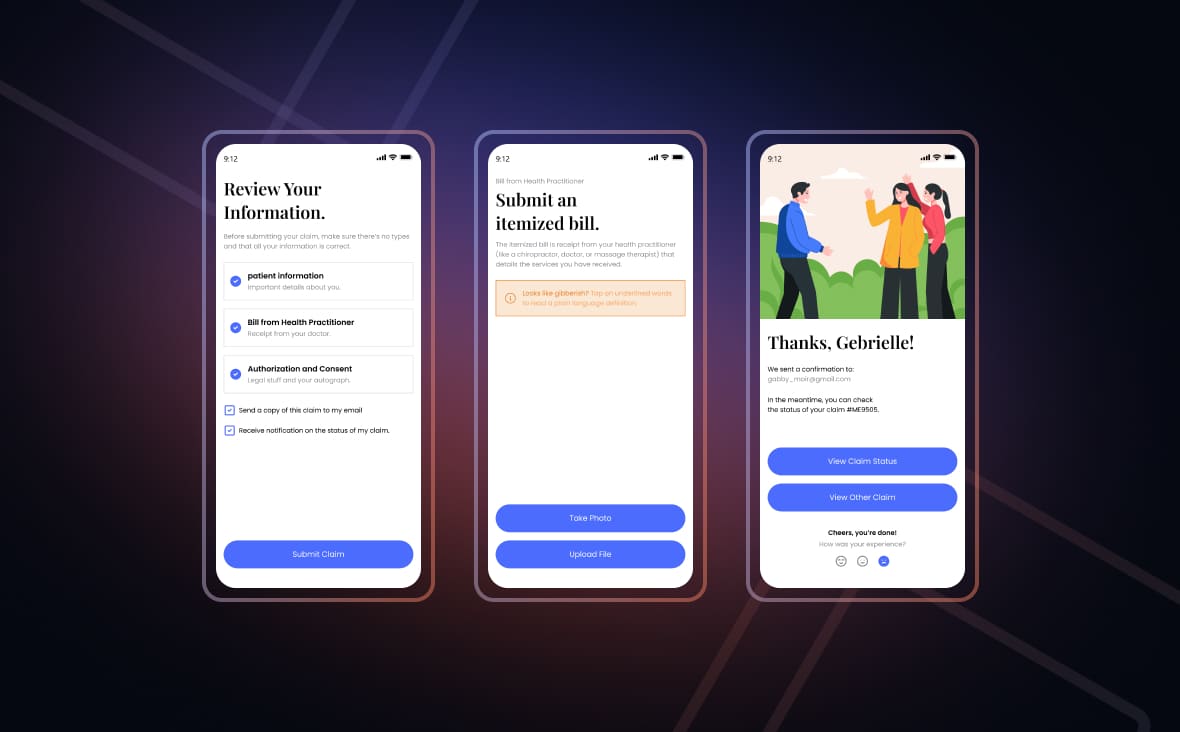
Prior Authorization App Development Features
Our prior authorization solution’s integration with EHR and EMR systems makes it easier for healthcare providers to view patient records.
As Knovator’s solution is integrated with billing systems, there is an assurance of accurate billing, much to the patient’s delight.
Our solution notifies healthcare providers of the status of requests made for prior authorization with timely alerts.
Here’s how we develop the Patient engagement solution
Reach out to us
- Searching for a robust telehealth app? Look no further than Knovator Technologies. We excel in transforming education business concepts into reality.
Understand & Evaluate Idea
- We understand and analyze your idea
- creating a strategic workflow
Sign NDA & Contract
- Upon signing the NDA and contract
- our team will promptly start the software development for you.
Prepare Plan
- Includes estimates
- budgeting
- and strategic planning for your innovative digital healthcare product
Start Working
- After you finalize the contract
- we’ll start working and bring your vision to life.
Our Happy Customers
Telehealth platform developed by Omniva Telehealth has been a pivotal move in our digital transformation journey. The platform's seamless scheduling and telehealth capabilities have not only enhanced patient satisfaction but also significantly improved operational efficiency. Also, the support team has been exceptional, ensuring a smooth transition and ongoing success.
Omniva has enabled us to expand our telehealth offerings. The platform's robust features and ease of use have allowed us to offer a wider range of services remotely, from mental health support to chronic disease management. Our patients appreciate the convenience and accessibility of our services, leading to higher engagement and satisfaction.
Frequently Asked Questions
It’s a system that streamlines the approval process for medical treatments, ensuring insurance coverage before procedures, reducing delays and administrative burdens.
Prior Authorization solutions optimize treatment planning, minimize claim denials, and enhance efficiency by ensuring treatments align with insurance guidelines.
Yes, our solution enables electronic submission of prior authorization requests, speeding up the process and promoting real-time communication between providers and payers.
In some cases, patients may need to provide consent or information, but our solution largely facilitates provider-payer communication to expedite approvals.
Yes, our solution is designed to integrate with multiple insurance companies, ensuring seamless communication and streamlined prior authorization processes across different payers.