Covid-19 has had a crushing effect on the US healthcare system, with healthcare leaders facing mounting pressure to reduce costs and mitigate losses. Add to that the workload placed on the staff and human error can escalate exponentially. However, despite the best efforts, the process of obtaining prior authorization is complex and time-consuming.
One failsafe way to reduce costs while easing the staff workload is by automating the prior authorization system. Especially for large hospitals and healthcare centers, manual prior authorization systems would require hundreds of dedicated employees and lead to major outsourcing expenses. A prior authorization solution increases the number of authorizations completed with less staff, along with ensuring accuracy throughout the process.
Why should you implement a prior authorization system?
An end-to-end automated prior authorization software pulls necessary data from your company’s EHR, creating a medical review within your case management system. The platform sends notifications of the patient’s care determination back to the EHR. Further, it also determines if authorization is required or if a medical necessity is needed. This improves the medical review process and frees the staff so that they can focus on patient care and complex high-risk accounts.
Prior authorization systems you should automate now
Medical necessity:
In the first place, your software should determine if authorization is required right away. Also, your vendor should be able to include commercial payers and easily upload content to EHR in order to discover LCD medical necessity requirements. Equally critical is the ability to use standard electronic transactions or payer website data for seamless cost-effective exchange between providers and payers.
Initiation:
As per a study, an average physician practice spends 13 hours of nursing time and 6.3 hours of clerical time for authorization. Automation can significantly reduce this time.
Find a hospital prior authorization system that can automatically initiate and receive authorization for scheduled services, submit inquiries and confirm prior authorization without human inputs. Make this your prior authorization strategy.
Notifications:
As a healthcare organization, you are required to notify insurance payers every time a new patient is admitted. In absence of automation, there are all chances of missing out on the one to two day notification period for payers to process an authorization record.
Automate admission notifications to eliminate the potential of missing out that window. The prior authorization solution also gives you access to payers that only take notifications through a web portal.
How can AI-powered prior authorization software lead to faster and better care?
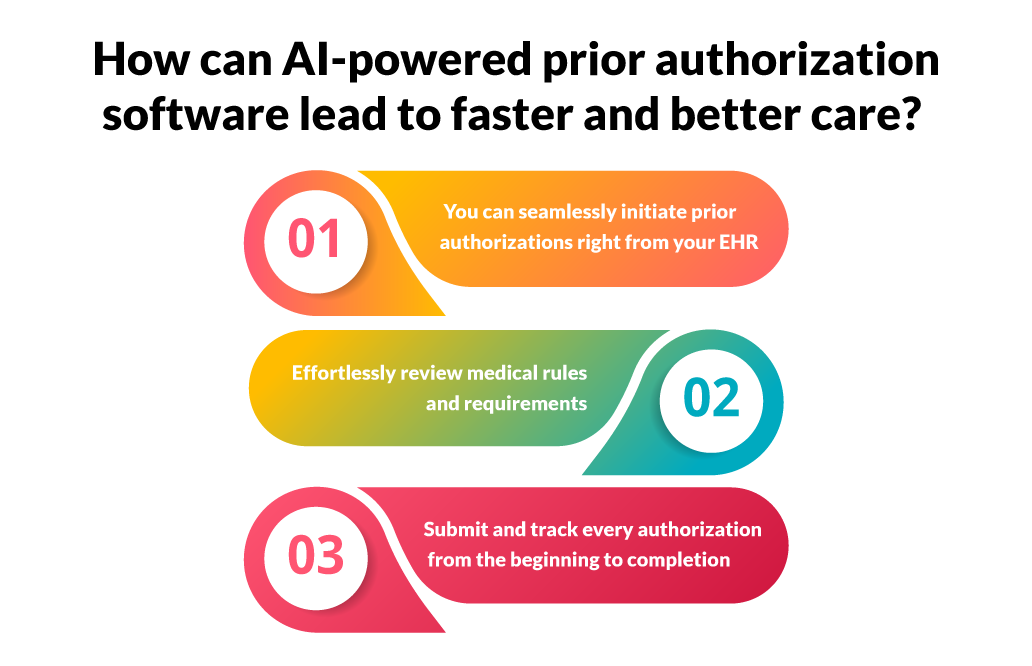 If you’re still over the edge, wondering whether to implement a hospital prior authorization solution in your healthcare organization, let’s see how it radically changes your prior authorization process.
If you’re still over the edge, wondering whether to implement a hospital prior authorization solution in your healthcare organization, let’s see how it radically changes your prior authorization process.
You can seamlessly initiate prior authorizations right from your EHR:
Without the prior auth software, physicians were forced to manually retrieve clinical notes and documents from electronic health records (EHRs). If relevant documents were unavailable, the case would be escalated to the nurse or physician who would provide the required documents.
To reduce waste and costs, hospitals need to address such operational inefficiencies. Automation is vital here.
When evaluating a prior authorization system, the first question to ask is how does the software handle clinical documentation. Knovator Technologies Prior Authorization Solutions integrates with your EHR. Automation fetches necessary medical history and patient information from your EHR, automatically populates required patient information and submits PA to the payer who receives a set of organized documentation meeting all of their requirements,
Automation collects everything needed for prior authorization approval at point-of-care, saving administrative time and resources.
Effortlessly review medical rules and requirements:
In the past, providers would manually comb through hundreds of payer forms and review the rules on the payer website, while constantly monitoring these websites for changes.
If the medical treatment is regularly administered, the prior authorization specialist would refer to a cheat sheet created with the payer’s rules and correct forms to complete. This method was time-consuming and prone to manual errors.
Staff could misinterpret rules and provide incomplete information to payers, leading to denials and expensive write-offs.
With a prior auth solution, teams do not need to hunt for payer rules or paperwork. Knovator’s Prior Authorization system keeps a track of all of this. It scasn the rules of thousands of health plans and gathers the information from the patient’s medical records in the EHR.
Submit and track every authorization from the beginning to completion:
Now, you could use robotic process automation (RPA) in this process to handle status checks. However, RPA has limitations. Bots would require custom builds and maintenance, leading to downtime whenever the EHR changes or website is updated. So if a task fails, human intervention would be needed.
In other words, the challenge of using RPA is that it would be limited to only simple and repetitive tasks.
Knovator’s prior authorization software offers an end-to-end hospital PA solution to help you submit and track every authorization from start to completion. The platform automatically performs status checks on insurance portals and alerts you when the authorization is approved. Thus, your staff can focus on patient care.
Automation with Knovator Technologies Prior Authorization Software leads to faster and better patient care
Automating the prior auth process becomes instrumental for healthcare organizations and hospitals since operational deficiencies can cost you revenue and patient leakage. Knovator’s prior auth system directly integrates with your EHR and frees up healthcare it solutions providers‘ time so that they can focus on patients. It increases operating efficiencies for both payers and providers.
 The benefits of a prior authorization system include faster prior auth submissions and decisions while reducing the turnaround time for patient care.
The benefits of a prior authorization system include faster prior auth submissions and decisions while reducing the turnaround time for patient care.
In a nutshell, Knovator’s prior authorization platform eliminates error-prone and time consuming manual work so that your prior auth team can focus on the health system to deliver faster and better patient care.