The prior authorization process is an important part of healthcare revenue cycle management and other administrative processes. It ensures high care quality and monitors costs and spending. However, the process to obtain a prior authorization is manual, time-consuming and creates a significant burden on administrative costs.
As per Becker’s Payer Issues website, 36% of rejected prior authorization requests are abandoned because it is a manual process especially when a non-electronic prior authorization is the need of the hour. Prior authorization processes are going to become more complex in the future. This calls for a paperless prior authorization system that is intelligently automated, AI-driven, and reduces the burden on healthcare administrative costs.
Let’s take a quick look at four key areas for automation in a prior authorization process:-
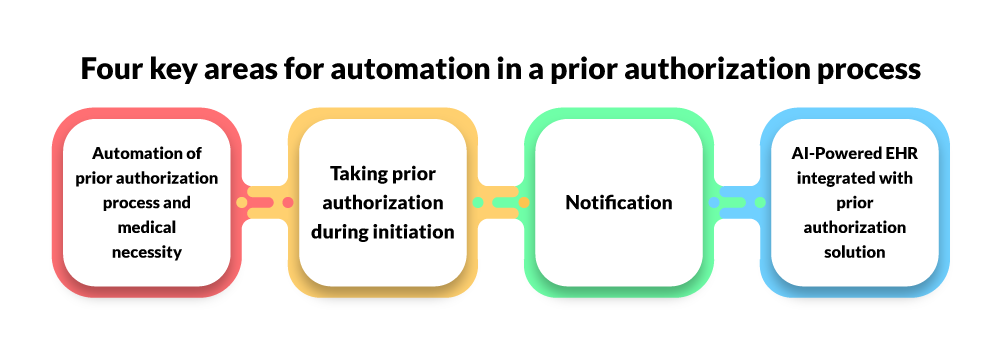
1. Automation of prior authorization process and medical necessity
Knovator Technology’s prior authorization solution automates this key area which includes determining if a particular payer supports standard electronic transaction or API or payer website data scraping to submit and receive prior authorization. It also determines if authorization is required at the claim submission or denial stage and ensures end-to-end automation. Alongside, it has a wide commercial payer network and helps in determining NCD medical necessity requirements.
2. Taking prior authorization during initiation
The complete prior authorization process is manual and keyboard-mouse driven. Software can automatically determine, initiate and obtain prior authorization for scheduled services without human intervention. It can also solve denials by adding a prior authorization number and re-submitting the claim to the payer.
3. Notification
Per process, a provider must notify a payer on patient admissions. It helps payers’ process authorizations on time. A prior authorization system should automate this step and notify a payer as soon as a patient is admitted. It also helps to divide and categorize payers that require web or call-based notifications to plan administrative work.
4. AI-Powered EHR integrated with prior authorization solution
Knovator Technologies has developed an AI-powered prior authorization solution that integrates with your EHR software. It pulls the necessary medical, clinical history, notes, and patient information from your EHR and finds the respective claim or initiates a fresh authorization by auto-populating data into the prior authorization system.
Authorization requests are submitted and tracked. Once a request is completed, it submits and populates a prior authorization number and other details like start and end date with procedure code to both the systems. Then, clinical documentation is added in a standard format in both the systems compatible with HIPAA and CMS guidelines.
Before selecting an area and vendor to automate manual prior authorization processes, you must consider the above points in your evaluation criteria.
Contact us for a prior authorization system to provide better and faster patient care.
We will now deep dive into nine major considerations that will help you evaluate solutions and pick the right prior authorization system.
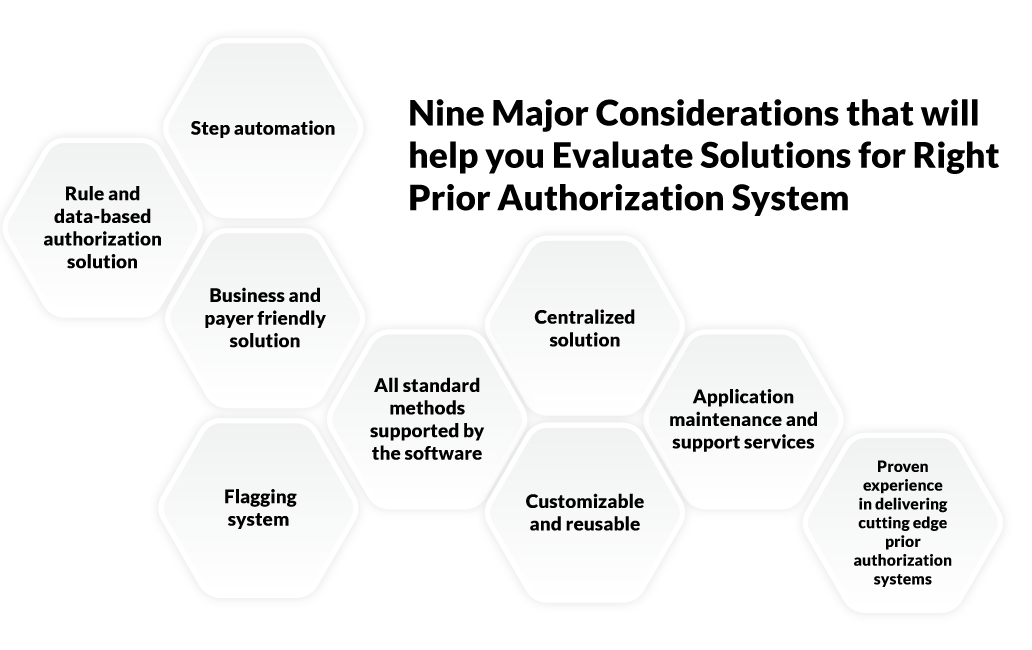
Step automation
You must evaluate and find the number of steps that a prior authorization system can automate. Right from determination, initiation, status tracking, submission, denial resolution, clinical intervention handling, exception handling to reporting, and a prior authorization solution must push only cognitive cases to the clinical team. It must automate every manual step and also report the accuracy of the solution that can be audited as and when required.
Rule and data-based authorization solution
Payers change their remittance and other contract rules based on geographical conditions. In the US, the payer rules differ state by state. Knovator Technology’s prior authorization system has a configurable rule system where business rules can be created and then configured based on changing requirements.
Any change in the rules requires re-configuring all the business parameters and a new rule related to the change and you are all set to perform authorization. This reduces the denial rate and also ensures the solution does not attempt authorization where it is not required. Software must have an integrated check to avoid denials based on medical necessity or pending documents.
Business and payer friendly solution
You can check if the software contains the updated information related to payers, CPT codes, modifiers, exceptions, and resolving authorizations as per the current prior authorization process and regulations
All standard methods supported by the software
Today, healthcare transactions between a payer and a provider are driven through EDI, API [Application Program Interface], HL7 feed, or process automation by robotic bots. You must ensure that the software supports all the above transaction types based on payer preference. For prior authorization, it must support the EDI 278 transaction.
Flagging system
If order changes post-authorization, Knovator Technology’s prior authorization solution will flag these cases and submit them to the staff for review, resubmit and get a clean claim.
Centralized solution
Ideally, you should not switch to multiple software for your EHR, practice management, RIS, prior authorization, and other business processes management. You must have a single login to access all the integrated applications.
If you’re looking to customize your prior authorization solution, call us!
Customizable and reusable
The software must be reusable and customizable to fit the needs of your organization and changes should cost you less.
Application maintenance and support services
Knovator Technology has a proven and certified team of support engineers to take care of regular maintenance and automate database transactions wherever necessary by setting up routine cron jobs. We have business expertise that can help you solve issues related to software dealing with prior authorization.
Proven experience in delivering cutting edge prior authorization systems
Knovator technology has proven experience in delivering prior authorization, EHR/EMR, and other healthcare systems which will help you get quality development and support at the best costs.
Also Read : Top Telehealth Business Ideas
Conclusion
With Knovator Technology’s prior authorization solution, you can run prior authorization processes at better costs and ensure timely payments, minimize denial, claim to rework, reduce claim rejections. Talk to our healthcare IT expert to create an automated and intelligent payment lifecycle solution that focuses on better health outcomes, improves patients’ satisfaction, streamlines workflows, and helps you run a lean and profitable healthcare business.
Get in touch with our healthcare IT experts to develop your prior authorization system.